Featured research
Prof. Jufen Liu's team published a paper in eClinicalMedicine revealing multimorbidity patterns increased risks of PD and PD-related functional degeneration among older adults

Introduction
Parkinson's disease (PD), aneurodegenerative disorder characterised by tremors and bradykinesia, has affected an increasing number of individuals from 2.5 million to 6.1 million during the past three decades. Previous research has indicated positive associations between certain chronic conditions, such as cardiometabolic diseases, arthritis, and depressive symptoms, and new-onset PD. Given the progressive nature of PD and the rapidly rising prevalence of multimorbidity, approximately one-third of adults worldwide exhibit two or more chronic diseases, further investigation of the association between multimorbidity and the onset of PD and its related functional degeneration is of substantial practical importance. Conducting comprehensive investigations into the association between diverse multimorbidity patterns, such as somatic and neuropsychiatric conditions, and new-onset PD also holds profound implications for developing clinical screening strategies targeted for PD.
First Affiliation: Peking University
First author: Ziyang Ren
Corresponding author: Jufen Liu
Journal: EClinicalMedicine, IF2023 = 15.1, CAS 1st Quartile
Citation: Ren Z, Xu Y, Sun J, Han Y, An L, Liu J*. Chronic diseases and multimorbidity patterns, their recent onset, and risk of new-onset Parkinson's disease and related functional degeneration in older adults: a prospective cohort study. EClinicalMedicine. 2023 Oct 6;65:102265. doi: 10.1016/j.eclinm.2023.102265.
Full Text Links: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10579290/
Abstract
Background: Certain chronic diseases contribute to increased risks of Parkinson's disease (PD), but the association between time-varying multimorbidity patterns and new-onset PD remains underexplored.
Methods: Data were from the Survey of Health, Ageing and Retirement in Europe (SHARE) waves 5-8 conducted between January 2013 and March 2020. Eleven chronic diseases were included, with ≥2 denoting multimorbidity. Three multimorbidity patterns were further defined: somatic multimorbidity (SMM), neuropsychiatric multimorbidity (NPM), and cardiometabolic multimorbidity (CMM). PD-related function degeneration included functional limitations, mobility limitations, depressive symptoms, and cognitive decline. Time-dependent analyses, competing-risk analyses, and mixed-effect models were utilised.
Findings: In this prospective cohort study, 557 developed new-onset PD during follow-ups among 64,273 participants included at baseline, as defined by participants' self-reported physician diagnoses. Participants with (vs. without) multimorbidity, SMM, NPM, and CMM were at 1.40-2.70 times higher PD risk after considering the competing role of all-cause death, which remained significant in all sensitivity analyses and were more pronounced in lower-income participants (P for interaction<0.05). Similarly, they tended to develop functional degeneration faster than those without these multimorbidity patterns (P < 0.05). Participants with recent-onset (newly diagnosed in 2015) multimorbidity patterns were at 1.45-3.72 times higher risk of PD than those never diagnosed. Interestingly, they were at comparable or even higher (though P values for >0.05) PD risk compared to participants with multimorbidity patterns diagnosed in 2013 or before. Furthermore, recent-onset (vs. prior diagnosed) NPM exhibited faster functional deterioration and cognitive decline (P for difference<0.05).
Interpretation: Our findings suggest that promoting early prevention of multimorbidity, especially recent-onset multimorbidity and NPM, could prevent some subsequent cases of PD and related functional degeneration among older adults. However, further studies are needed to confirm this association.
Dr Jufen Liu and her colleagues from School of Public Health, Peking University use a large cohort study in Europe to explore multimorbidity patterns and new-onset Parkinson's disease (PD).
In this study, we utilised data from the Survey of Health, Ageing and Retirement in Europe (SHARE), which is a multicentre panel survey covering community-dwelling individuals aged 50 years and above across twenty-seven European countries and Israel. Our analysis utilised SHARE waves 5–8 conducted between January 2013 and March 2020.12, 13, 14, 15 The baseline was set as wave 5, with follow-ups in waves 6–8 conducted starting in 2015, 2017, and 2019. Eleven chronic diseases, including hypertension, iabetes, dyslipidaemia, heart diseases, stroke, lung diseases, digestive diseases, cataracts, rheumatoid arthritis or osteoporosis, affective disorders, and dementia, were defined by participants’ self-reported physician diagnoses or treatments at each wave. Of them, affective disorders and dementia were further classified as neuropsychiatric diseases, while others were classified as somatic diseases. Hypertension, diabetes, dyslipidaemia, heart diseases, and stroke were further classified as cardiometabolic diseases. Multimorbidity referred to the coexistence of two or more chronic diseases; somatic multimorbidity (SMM) included the coexistence of two or more somatic diseases; neuropsychiatric multimorbidity (NPM) involved the coexistence of both affective disorders and dementia; and cardiometabolic multimorbidity (CMM) encompassed the coexistence of two or more cardiometabolic diseases.
A total of 64,273 participants (44.5% men) aged 66.0 (59.0–74.0) years were included. Over approximately six years of follow-up, 557 participants (175.3/105 person-years) developed new-onset PD, while 9146 (2471.9/105 person-years) participants died. Participants who had multimorbidity, SMM, NPM, or CMM at baseline seem to be at higher risk of new-onset PD (all P values < 0.05). Fig. 1 shows that participants with NPM and dementia at baseline exhibit the highest incidence density of PD and all-cause mortality.

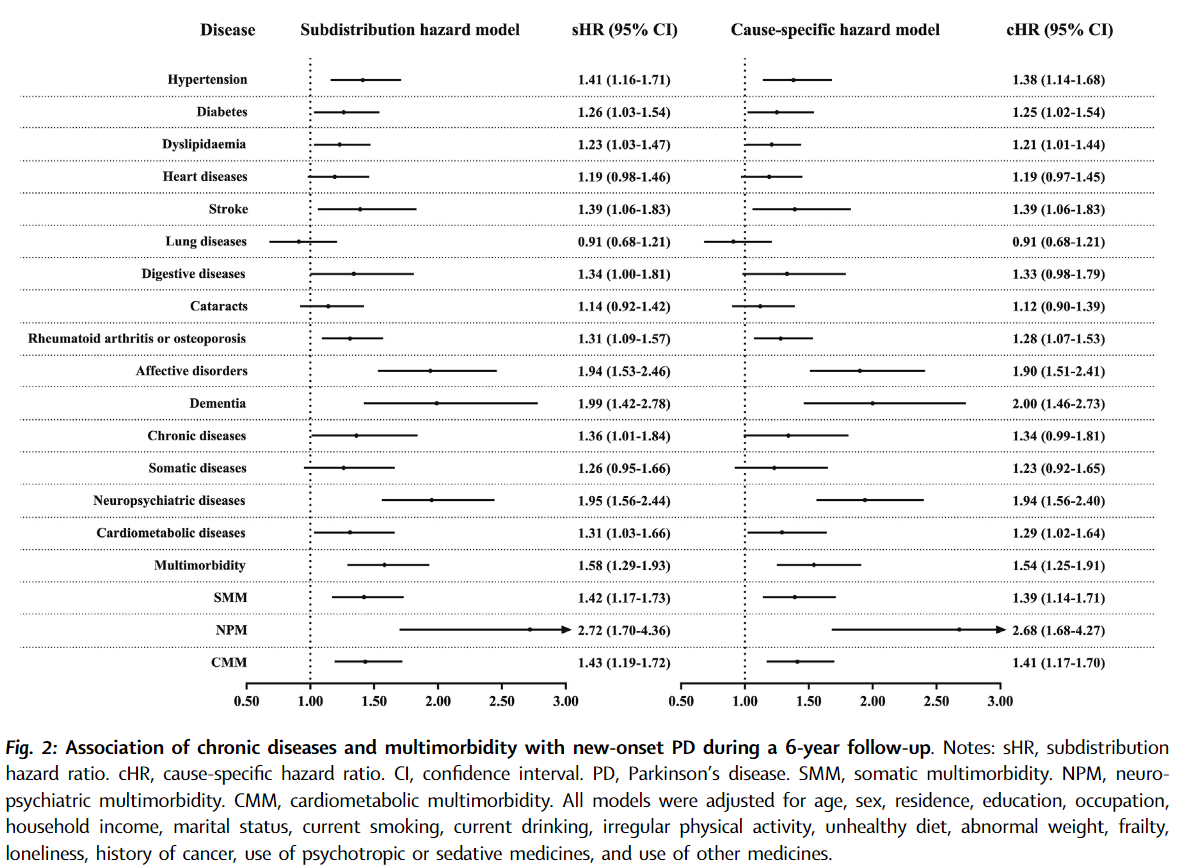
Competing-risk analyses based on subdistribution and cause-specific hazard models were used to explore the associations of chronic diseases and multimorbidity patterns in 2013 with new-onset PD during 2013∼2019, respectively, with all-cause death as the competing event. The cause-specific hazard model and subdistribution hazard model are typically utilised to deal with competing risks. Furthermore, time-dependent analyses on time-varying exposure variables (i.e., chronic diseases and multimorbidity) were conducted to capture the changes in chronic conditions in older adults during follow-ups. Six sensitivity analyses were conducted to ensure the reliability of our conclusions: First, complete-case analysis without multiple imputation; Second, excluded participants with heart diseases or stroke at baseline or during follow-up to rule out the vascular causes of parkinsonism; Third, excluded participants with dementia at baseline or during follow-up to avoid misdiagnosing dementia as PD; Fourth, defined new-onset PD strictly (i.e., the following situations exist simultaneously: self-reported physician diagnosis, at least one limitation in ADLs, IADLs, and mobility, depressive z scores of >1.5, and cognitive z scores of <−1.5); Fifth, excluded patients diagnosed with PD in 2015 to account for potential latency time windows and avoid the potential reverse-causality bias; Sixth, further considering countries and survey weights to ensure that the conclusions can be extrapolated from the analytic sample to the population.
According to Fig. 2, participants with certain chronic diseases, such as hypertension, diabetes, dyslipidaemia, stroke, rheumatoid arthritis or osteoporosis, affective disorders, and dementia, are at higher risk of PD, compared to those without corresponding diseases. Those with (vs. without) multimorbidity, SMM, NPM, and CMM are at around 1.40–2.70 times higher risk of new-onset PD, with similar values of sHRs and cHRs. At the same time, participants with NPM and dementia seem to exhibit the highest PD risk. In all the sensitivity analyses, the associations between multimorbidity and new-onset PD remain significant, though the association between certain chronic diseases and new-onset PD vary.
According to Table 3, recent-onset multimorbidity, SMM, NPM, and CMM are significantly associated with increased risks of new-onset PD, with sHRs (95% CIs) of 1.75 (1.23–2.48), 1.45 (1.01–2.06), 3.67 (1.90–7.12), and 1.58 (1.10–2.26) and cHRs (95% CIs) of 1.75 (1.23–2.48), 1.45 (1.02–2.06), 3.72 (1.89–7.31), and 1.58 (1.11–2.25). Although the sHRs and cHRs between prior diagnosed and recent-onset groups appear comparable, and the latter seems more significant, the P values for differences between them are not statistically significant (all >0.05). In addition, only participants with recent-onset diabetes and rheumatoid arthritis or osteoporosis are at significantly higher risks of PD compared to those with prior diagnosed corresponding conditions (P values for difference<0.05).

To our knowledge, this is the first and most comprehensive population-based cohort study to investigate the associations of chronic diseases, multimorbidity patterns, and their recent onset with new-onset PD and PD-related functional degeneration. The time-dependent analysis used in this study helps capture the time-varying chronic conditions of older adults more accurately. The competing-risk analyses based on subdistribution and cause-specific hazard models and mixed-effect models with random intercepts and slopes used in this study ensure the precision of our research methodology. Our findings call for early detection and effective management of multimorbidity in the prevention of PD and functional degeneration, especially for old adults with recent-onset neuropsychiatric multimorbidity. Furthermore, more diverse instruments beyond functional degeneration are warranted to capture PD risk exactly.
Funding
The National Key Research and Development Program, Ministry of Science and Technology, China; Zhongnanshan Medical Foundation of Guangdong Province; Major Project of the National Social Science Fund of China; Fundamental Research Funds for the Central Universities.
Author Biography
First author
Ziyang Ren, Ph.D. Candidate, Institute of Reproductive and Child Health, School of Public Health, Peking University.
Research Interests: Application of life course epidemiology in the study of middle-aged and elderly health. To date, several papers have been published as the first author in eClinicalMedicine (Impact Factor = 15.1), JAMA Network Open (Impact Factor = 13.8), General Psychiatry (Impact Factor = 11.9), and Globalization and Health (Impact Factor = 10.8) and so forth.
Corresponding author

Dr. Jufen Liu, Assistant professor (Tenure Track), Institute of Reproductive and Child Health, School of Public Health, Peking University.
Dr. Jufen Liu lead her research to investigate the early life determinants and trajectories of chronic diseases throughout the life course, through which to develop population level interventions to prevent chronic diseases and multimorbidity, as well as to support translation of discovery into policy and practice both within in China and in the global community. She has a broad interest in birth defects and disability, focusing on neurodevelopmental disorders, degenerative diseases, chronic diseases and multi-morbidities at all ages. She has led on original research articles and her publications are featured in journals such as International Journal of Epidemiology, eClinicalMedicine, Social Science and Medicine, Globalization and Health, General Psychiatry, Chinese Journal of Epidemiology, Chinese Journal of Preventive Medicine, and so forth. Her research has been recognized with awards from Huaxia Medical Science and Technology Assiociation, Chinese Preventive Medicine Association, Beijing Preventive Medicine Association and Ministry of Education, China. Dr Liu served as scientific communities, she is a standing committee member of the China Maternal and Child Health Association's Professional Committee on Perinatology and Metabolism; a member of the Chinese Preventive Medicine Association's Professional Committee on Birth Defects Prevention and Control, and the Committee on Family-School-Community Education of the Chinese Family Education Society. She is also served in the editorial boards of academic journals, including Reproductive Health (Deputy Editor), BMC Pregnancy and Childbirth (Editorial Board Member), China CDC Weekly (Guest Editor), Frontiers in Nutrition (Guest Editor), Nutrients (Guest Editor), and China Journal of Reproductive Health (Editor).
Contributed by | Dr. Jufen Liu and her research team (Peking University)
Reviewed by | ExposomeX Team
Institute Introduction

Peking University Institute of Reproductive and Child Health
Peking University Institute of Reproductive and Child Health mainly focus on the research areas of reproductive health epidemiology, environment and reproductive health, and translational research in reproductive health studies. It particularly focuses on the distribution patterns, influencing 叶酸ctors, mechanisms of disease, and prevention strategies for adverse reproductive health outcomes, utilization of big data in reproductive health, application of artificial intelligence, and related interdisciplinary transformations. The institute serves as the direct support unit for the NHC Key Laboratory of Reproductive Health (Peking University) and is specifically responsible for the National Office for Maternal and Child Health Annual Report. Its achievements have been published in top international journals such as NEJM、Lancet、JAMA、BMJ、Cell、PNAS、Science Bulletin、Lancet subsidiaries, Science subsidiaries, Nature subsidiaries, The Innovation, Environ Health Perspect, Environ Sci Technol, etc. It also hosts the core Chinese scientific journal "Chinese Journal of Reproductive Health" (Website: http://cjrh.bjmu.edu.cn/).
The outstanding talents at home and abroad are welcome for seeking job and build dream here. Contacts: Bin Wang, Vice Dean of Institute of Reproductive and Child Health of Peking University. Main page: https://sph.pku.edu.cn/info/1442/4225.htm